Latest Articles
 6 Min Read
6 Min ReadSpotlight On: Harman Johal, Wealth Management Regional Executive, U.S. Bank
July 2025 — In an interview with Invest:, Harman Johal, wealth management regional executive at U.S. Bank, said that Houston’s diversification and strategic growth make it an ideal location for expanding wealth management services. “This economic diversification has brought in a wide array of businesses, and as businesses relocate, so do their support services, including banking and wealth management.” What makes Houston an ideal location for U.S. Bank’s operations, particularly...
Latest CEO Articles

‘Patience Grasshopper:’ The Power of Patience and Team Trust
“Patience, grasshopper,” as the famous quote from the 1970s TV series Kung Fu goes. My dad used to quote this to me as a
I:BSSAll Markets
caa takes a deep dive into the markets we cover through our on the ground approach. See why you should be doing business in the markets we cover now.

The Regional Economic Sentiment Index, drawn from the Invest: Business Sentiment Survey, tracks perceptions of economic strength across 20 U.S. metro areas. The index is based on a standardized question posed to senior executives and public officials featured in Invest: reports, asking them to rate the strength of their regional economy on a scale of 1 to 5.
The 2Q25 survey revealed a modest decline in regional economic sentiment, driven by rising uncertainty, elevated costs, new tariffs, and the absence of interest rate cuts. Business leaders, particularly in the Northern region, expressed growing concern about the macroeconomic outlook, marking a shift from the optimism seen earlier in the year.
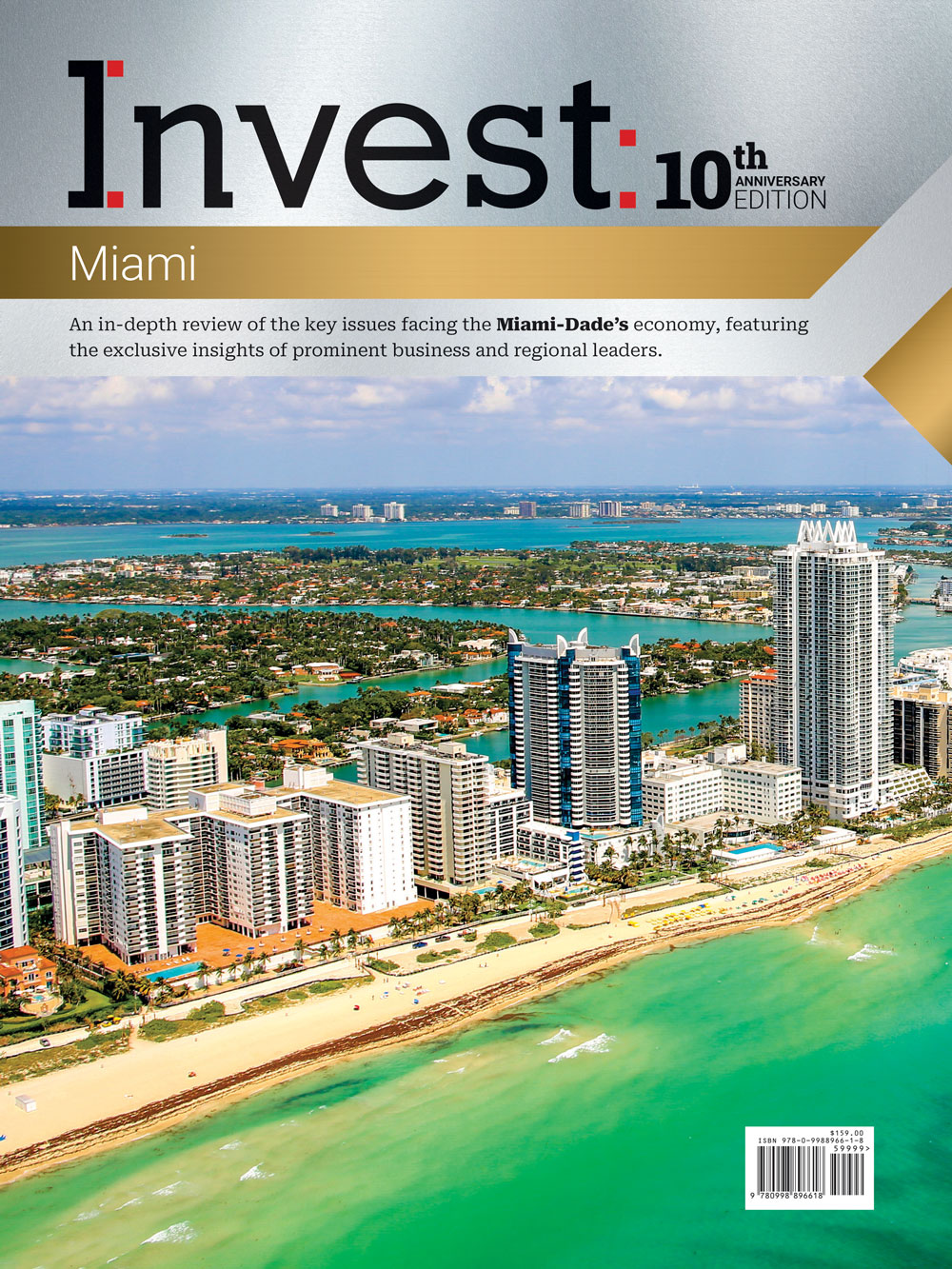
Explore our latest reports
caa annual business guides take a 360° view of each metro area we cover through in-depth analysis, interviews with local business and political leaders and comprehensive data and statistics. Click on a cover to read more.
Invest:Insights
Invest:Insights captures the collective voice of the business community. This video series features industry leaders, executives, and entrepreneurs sharing insights on key sectors and local economic opportunities.
C-Suite Executives & Industry Leaders Attend Annually
Access
Exclusive Panels and Keynotes
Industries Represented
Leadership
Summits
caa hosts exclusive VIP conferences and events where C-suite executives convene to discuss key opportunities and challenges facing their markets, forging a stronger foundation for building business.
About caa
caa is an integrated media company that connects the dots in the markets it covers, providing business intelligence to businesses, executives, investors, and entrepreneurs across its digital and print platforms. It produces annual economic reports and engaging content on important US metro regions, while forging strategic connections through its conferences and events.